Although the probability of OA from history cannot be accurately quantified, a typical history and consistent exposure could lead to a high pretest probability (eg, > 70%) before additional investigations are performed. This pretest probability influences the posttest probability of OA after the performance of subsequent investigations such as methacholine challenge and/or the assessment of the relationship of specific IgE to a work allergen, when feasible. Conversely, a paucity of suggestive factors from history (eg, pretest probability of OA of around 15%) will result in a low posttest probability of OA, even when the results of other investigations are positive. 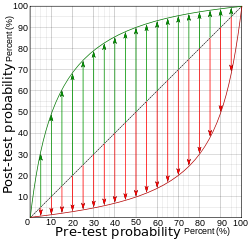
subscribe on our Facebook Canadian Health and Care – https://www.facebook.com/pages/Health-and-Care-Info/963724666987760
The incorrect diagnosis in 26% of suspected cases of sensitizer-induced OA from history alone compared with SIC (in a compensation referral series), emphasizes the importance of the further assessment of those with a positive history of OA in order to avoid unnecessary job change. Although further diagnostic testing should always be attempted, the correct diagnosis in almost 75% of patients based on history alone also demonstrates the importance of a careful history and that occasionally the history (among those with asthma) may be sufficient to diagnose OA, especially in cases of irritant-induced OA. Thus, the history has high sensitivity, and without an appropriate medical history the patient is unlikely to undergo the objective tests needed to make the correct diagnosis.
Panel Consensus
1. In all individuals with new-onset or worsening asthma, take a history to screen for WRA (OA and WEA). Then confirm the diagnosis of asthma and investigate to determine whether the patient has WRA, whenever possible performing these tests prior to advising the patient to change jobs.
2. In all individuals with suspected WRA, obtain a history of job duties, exposures, industry, use of protective devices/equipment, the presence of respiratory disease in coworkers, and consult MSDSs, which list many recognized hazardous agents. Document the onset and timing of symptoms, medication use, and lung function, and their temporal relationship to periods at and away from work.